Transvaginal Mesh Complications
It sounds like the script of Hollywood’s latest horror movie: a woman enters the hospital for a simple surgical procedure, and leaves with something inside her that will cause terrible pain, organ damage, and possibly permanent injury. Unfortunately, it’s no movie script – it’s reality for thousands of women around the U.S. who are suffering from vaginal mesh complications.
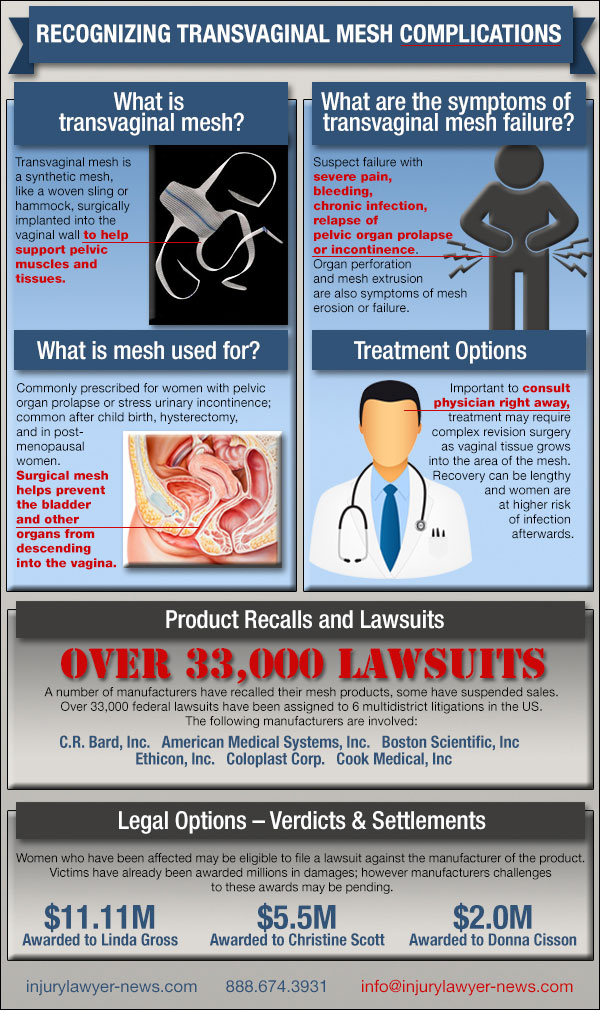 Since the introduction of transvaginal mesh in the 1990s, millions of women have undergone vaginal mesh surgery as an easy fix for pelvic organ prolapse (POP), stress urinary incontinence (SUI) and other conditions. But it has since came to light that mesh manufacturers, including Johnson & Johnson, AMS, Coloplast and Boston Scientific, were less than forthcoming about the risk of serious device complications, which reportedly affect 10 percent of all recipients.
Since the introduction of transvaginal mesh in the 1990s, millions of women have undergone vaginal mesh surgery as an easy fix for pelvic organ prolapse (POP), stress urinary incontinence (SUI) and other conditions. But it has since came to light that mesh manufacturers, including Johnson & Johnson, AMS, Coloplast and Boston Scientific, were less than forthcoming about the risk of serious device complications, which reportedly affect 10 percent of all recipients.
The FDA has since stepped in, deeming surgical mesh problems “not rare,” and warning that mesh products may be no more effective than other, safer treatment options.
Common vaginal mesh complications
The most serious surgical mesh complications are due to vaginal mesh erosion, also known as extrusion or protrusion. Erosion occurs when the mesh implant does not remain secured in place, and instead protrudes into the vaginal wall. This can cause tissue damage and the mesh may actually become visible in and around the vagina.
Transvaginal mesh failure, including erosion, affects approximately 10 percent of all patients within a year of their initial surgeries. As the mesh erodes, it can lead to other, very serious complications – painful intercourse, chronic infection, and perforation of other organs, including the bowels, bladder and rectum. Even with multiple revision surgeries, there is no guarantee that internal damage from vaginal mesh can be repaired.
Women suffering from transvaginal mesh complications may experience:
- Transvaginal mesh failure: When transvaginal mesh surgery fails, or vaginal mesh does not correct a condition, or when other surgical mesh problems arise, revision surgery may be required.
- Mesh extrusion or erosion: Transvaginal mesh may erode, or drift into the vaginal wall. Requires revision surgery.
- Vaginal shrinkage: Failed mesh may shrink, forcing the vaginal wall to shrink. This may cause serious tissue damage, and can make sexual intercourse impossible.
- Vaginal scarring: Mesh erosion may result in internal scarring of the vagina.
- SUI or POP: Though surgical mesh is intended to treat stress urinary incontinence (SUI) and pelvic organ prolapse (POP), it can actually cause these conditions to occur, either as new conditions or as relapse.
- Dyspareunia: This condition relates to vaginal pain, usually during intercourse, but can also occur during other types of penetration, such as insertion of a tampon.
- Sexual pain in men: Men may experience pain during intercourse with a woman whose mesh has extruded, or migrated out of position.
- Rectocele: Though vaginal mesh is intended to correct rectocele, or bulging rectum, it may actually worsen the condition.
- Organ perforation: When transvaginal mesh migrates out of place, it may protrude through the vaginal wall and puncture adjacent organs, including the bladder, rectum, and the bowels.
- Chronic infection, including UTIs: Transvaginal mesh failure may cause persistent infection around the implant site. Women may also experience urinary tract infections (UTIs) and bladder infections.
- Extreme pain: Many complications bring with them excruciating pain, both during normal activity and during sexual intercourse. Prolonged or sustained bleeding may also occur.
Relapse of POP and SUI
One of the ironies of vaginal mesh is that the product can cause the very conditions it was intended to treat. Most women choose transvaginal mesh as surgical repair for pelvic organ prolapse (POP) or stress urinary incontinence (SUI). POP occurs when the pelvic or vaginal muscles weaken or collapse, allowing internal organs to protrude into the vaginal wall. SUI is a type of incontinence common in aging women and women who have given birth.
In both cases, vaginal mesh is intended to strengthen the vaginal wall muscles, providing relief of these symptoms. Unfortunately, surgical mesh has been shown to aggravate both conditions, causing a relapse of POP and SUI. Additionally, some women have developed POP or SUI for the first time – after receiving transvaginal mesh. Corrective transvaginal mesh surgery is needed to further address these mesh problems.
FDA warnings concerning mesh complications
The FDA first approved surgical mesh in the 1990s. The products, which are manufactured under various brand names by several companies, quickly rose to popularity, as vaginal mesh was marketed as a better, more effective solution to treat POP and SUI.
However, in October 2008, the FDA released a Public Health Notification, warning consumers that the agency had already received more than 1,000 adverse event reports. The notification warned of “serious consequences,” specifically “erosion through vaginal epithelium, infection, pain, urinary problems, and recurrence of prolapse and/or incontinence.” There were also reports of bowel, bladder, and blood vessel perforation during insertion. In some cases, vaginal scarring and mesh erosion led to a significant decrease in patient quality of life due to discomfort and pain, including dyspareunia.
In 2011, the FDA issued an updated Safety Communication, stating that, “serious complications associated with surgical mesh for transvaginal repair of POP are not rare… Furthermore, it is not clear that transvaginal POP repair with mesh is more effective than traditional non-mesh repair in all patients with POP and it may expose patients to greater risk.”
Medical studies & treatment
In addition to data collected by the FDA, medical studies have been conducted into the prevalence of transvaginal mesh complications. One study, which reviewed information from 12,000 mesh recipients, revealed that 10 percent had experienced mesh failure.
Another study, which was presented at the European Association of Urology Congress in March 2013, revealed that a woman’s age and other factors may contribute to her risk of complications. Data included information from 667 women who had undergone mesh surgery between 2006 and 2010. More than 17 percent experienced some type of complication, including 32 women (almost 5 percent) who had reported vaginal mesh erosion.
In many cases, revision surgery is the only recourse for serious complications from vaginal mesh. Unfortunately, surgical correction is not effective in all cases, and some damages may be permanent.
Resources
- Common Health, Surgeons Challenge FDA Warnings On Vaginal Mesh http://commonhealth.wbur.org/2011/08/surgeons-challenge-fda-warnings-on-vaginal-mesh
- FDA, Public Health Notification: Serious Complications Associated with Transvaginal Placement of Surgical Mesh in Repair of Pelvic Organ Prolapse and Stress Urinary Incontinence http://www.fda.gov/medicaldevices/safety/alertsandnotices/publichealthnotifications/ucm061976.htm
- FDA: Urogynecologic Surgical Mesh Implants http://www.fda.gov/MedicalDevices/

